Erica LeCounte, MPH
Population Health Service Fellow
City of Milwaukee Health Department
Center for Urban Population Health
Milwaukee, Wisconsin
When did you begin your fellowship?
July 1, 2012
Where is your fellowship
placement?
I’m placed with the City of Milwaukee
Health Department and the Center for Urban Population Health.
What projects are you currently
working on?
I’m currently working on four main
projects:
1) I’ve been developing an evaluation plan for the DAD Project, a
new home visiting program for fathers with young children or men in a father
role. I’ve been researching and designing surveys and evaluation
tools to measure outcomes, and I will also be facilitating focus groups with
mothers and fathers to get feedback about the program.
2) I am also working on a home visiting evaluation to see how well
the Empowering Families of Milwaukee, Nurse Family Partnership, and Prenatal
Care Coordination programs are doing in helping mothers have healthy
pregnancies and healthy children. So far I have been working on an
IRB application and will soon begin analyzing program data.
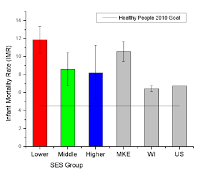
3) I am working to develop a prematurity surveillance system and
analyzing data to get a better understanding of premature births in Milwaukee.
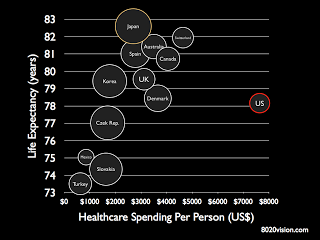
4) Finally, I am working on a life expectancy project, which
involves calculating and mapping life expectancies for all zip codes in Milwaukee County.
Why did you decide to pursue a career
in public health?
I took a course in undergrad in
maternal and child health. The course introduced me to public
health, and I realized that there are other ways of improving health than
becoming a physician. I also learned a lot about developing programs
and evaluation plans, which really introduced me to the field of public health
and made me want to pursue a career in this area.
What
made you decide to join the fellowship program as opposed to other career or
educational options?
I chose the fellowship because I had
spent my entire life in school and I wanted more work experience, which I knew
I would need for the jobs I am interested in pursuing. I also
thought the fellowship would be a great opportunity to grow and develop in ways
that I wouldn’t be able to if I had stayed in school for another degree or
accepted a job right out of grad school.
What has been your favorite part of
the fellowship so far?
The ability to explore different
career options. My background is in epidemiology, so in my first
year I focused mostly on projects involving data. In my second year
I have been able to focus more on planning, implementing, and evaluating
programs. It has helped give me a broader range of experience and a
better idea of what I want to do career-wise.
What is one of the most important
things you have learned over the course of your fellowship so far?
Definitely to take advantage of every
opportunity I’m given and utilize the people around me. It’s great
to be able to take advantage of my preceptors, especially when I have questions
about any ideas I have or about different career paths.
If you could travel anywhere in the
world, where would you go and why?
This is a hard question for me –
there are so many places I want to go! I guess I’d say Hawaii because
it would be great to take a nice long vacation on the water.