Carly Hood, MPA, MPH
Population Health Service Fellow 2012-2014
Wisconsin Division of Public Health
Health First Wisconsin
Wisconsin Center for Health Equity
Madison, WI
As I wrap up my final week as a Wisconsin Population Health
Service Fellow, not only am I dedicating time to ensuring projects are complete
and my desk(s) are clean, but I’m making time to reflect on what the last 2
years as a fellow (and 4 as a Wisconsin citizen) have meant to me. I moved here in the summer of 2010 as a
reverse-culture-shocked graduate student, ready to apply what I had most
recently seen in Vietnam as student of public policy at the
Robert M. LaFollette School of Public
Affairs. As a “fighting Bob” I took classes in public management, policy
analysis, policy-making process and advanced statistics. And ate it up! I can
see now, I was most definitely at a point in my life where school sounded right
(boy, that ship has sailed!) But it was here that I also began seeing my lens
take shape, my interests honed. I observed that the policies I chose to
analyze, the experiences I brought to class to discuss, and the data I wanted
to play with focused on health and access to what I had always seen as a human
right: opportunity to live a healthy life. I quickly learned about the dual
program with the
UW School of Medicine and
Public Health and added on an extra summer of epidemiology, social and
behavioral health, and health policy courses to obtain my Master of Public
Health and Global Health Certificate alongside my Master of Public Affairs
degree.
I was fortunate to have been told about the
fellowship
program early enough to apply and post-application submission, waited
anxiously to hear back from folks at the
Population Health Institute.
Finally, in late February, I received the call that helped shape my career path
and joined the 4 other fellows in my cohort summer of 2012. Since my graduate
research was based on food policy, I naturally found dual placement sites at
the
Division of
Public Health in the Chronic Disease Program and at
Health First Wisconsin. (I later added
my tri-placement at the
Wisconsin Center for
Health Equity). And then…Poof! 2 years disappeared!
As my fellowship is ending soon, I was recently asked, “What
do you think you’ve done as a fellow?” Wellllllllll (insert headscratch). Sometimes
I want to say, “What HAVEN’T I done?!” Other times I ask myself, “Have a done
ANYthing?” For most fellows, I believe it’s a difficult question to answer when
there aren’t particular milestones, expectations or deliverables like those
found in many other public health positions descriptions (besides the CALs of
course!) The concrete products of my fellowship (which I was interested in
hearing 2
nd year fellows talk about as an applicant and incoming fellow
so I’ll touch on here) are what I shared in my exit interview last week and
include the following: I developed 2 strategic evaluations both aimed at
increasing capacity for folks working with homeless, impoverished and/or
jobless individuals; I designed and implemented a year-long health equity
training at both placement sites; I analyzed socioeconomic data for a chapter
in the 2014
Healthiest Wisconsin
2020 Baseline and Health Disparities Report; I published
1
paper (2 in the works yet!), 2 Opinion pieces and 4 Letters to the Editor
in various Wisconsin media outlets; I led 2 years of discussion courses for
undergraduates interested in public health; I trained local and tribal health
departments around the state on the use of
national community health
tools; I presented on health equity/social policy in public health to
community groups, students, state public health employees, and national
audiences; and I developed
bi-monthly
resources on health equity and social policy for national partners.

While most of these have a tangible item attached to them (a
pdf report, a powerpoint presentation, a word document newsletter), some of
them do not. And in my eyes, the more important outcomes of all of these
projects have very little to do with the items one can see and touch. I have
found much more value in the relationships I’ve developed, the heightened understanding
of how public health & policy works at a State Health Department AND an
advocacy organization, and the confidence that my perspective is a valued and
impactful one.
I don’t believe in fate. I don’t think my career ‘required’
this 2-year experience or that I couldn’t also have been happy and successful
in another position (there are certainly positives and negatives to this
position). But I do believe that this experience gave me the flexibility and time to explore the many facets of public health, the plethora of
partners who are involved, and the varied organizations that support the field
of public health. I believe I was fortunate to be given the opportunity to hone the skills I wanted
and dump those I wasn’t interested in. And as an academically funded staff
person working in the field, I had access to more resources and training alternatives that helped me sharpen a sort
of ‘field of expertise.’
The fellowship was a great opportunity. And—like everything
else—it came with a fair share of challenges. I dealt with a loss of preceptors
(2 of mine left in the middle of my fellowship). I was conflicted with 2
placement sites and not feeling 100% a part of either. I was challenged to
assert the understanding that ‘fellow’ does not mean ‘student’ or
‘administrative assistant’—we are in fact highly trained professionals seeking
mentorship and experience early in our careers. And lastly, I struggled with
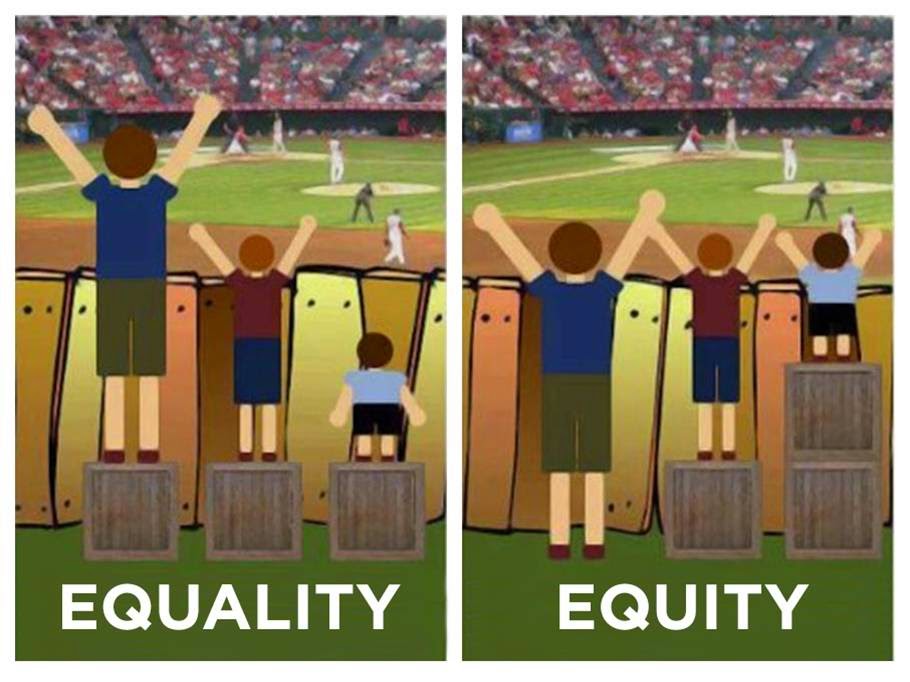
evolving interests, being originally interested in food policy my interests broadened
from issues of healthy food access to more upstream equity associated with
income, education and housing. That made projects at my particular placement
sites hard to find at times…but my preceptors were flexible and encouraging and
I was able to develop my own projects that focused on equity and increasing
capacity within my placement institutions. I was also able to expand many of my
projects to the
Wisconsin Center for Health
Equity, where I revamped the website and built several partnership that
results in facilitation and keynote speaking engagements.
In this way, the fellowship demanded innovativeness and
honesty. I had to be cognizant of the skills and abilities I wanted to develop, I had to be honest and open about those, and
then look for ways to infuse that work where I & my organizations were. In
contrast to many other positions, I had to speak up louder than I might
otherwise and was forced to be my own advocate. While this can be challenging at
first, it ultimately helped me learn who I was, what I wanted, and encouraged
me to think outside of the box. Today I feel lucky to have had the chance to
say, “Hey! This is what I want to
work on. How do we make that happen?”
In looking back over the last 4 years—and the fellowship in general—Wisconsin has provided a safe space for me to overcome my
reverse-culture shock, make new friends and professional connections, and build
on the amazing efforts of places like the
policy school (3
rd in the
country for Social Policy!), the
Institute for Research on Poverty, the
Population Health Institute, and the
School of Medicine & Public Health.
Due to its size and approachability (plus people’s lovely Midwestern demeanor!)
Wisconsin is a ripe place for networking and building connections. I will miss
those that I’ve made as I move on to a new position as Clinic & Public
Health Director for a
small clinic—in
a new country! But I feel more equipped to deal with the challenges I will
likely face in the developing world, and look forward to contrasting the public
health system in Belize with that of the United States and Wisconsin. Thank you
to the fellowship community for the support and learning you’ve provided me!!!!
I do hope you’ll keep in touch.