Leslie Tou, MPH
Population Health Service Fellow, 2nd Year
Wisconsin Department of Health Services
UW-Madison Lifecourse Initiative for Healthy Families
Madison, Wi
I’m angry.
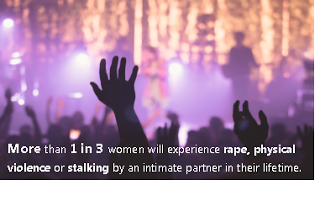
Honestly, we- as public health professionals, as citizens, and as human beings- should all be angry. Lately, it seems like we actually need a reminder that women still experience violence at an alarmingly high rate. Between Russia decriminalizing domestic violence and Trump’s new budget threatening to completely eliminate all Violence Against Women Act (VAWA) grant programs, you could be forgiven for thinking maybe it’s not an issue anymore. But the numbers don’t lie. 1 in3 women and girls across the globe experience gender-based violence [*] (1). That is over 30% of our world’s women and girls who will experience sexual, physical and other abuse in their lifetimes. Here in the United States, more than 1 in 3 women have experienced “rape, physical violence, and/or stalking by an intimate partner in their lifetime” with 1 in 4 experiencing severe intimate partner violence. And nearly45% of all American women (almost 1 in2) have experienced sexual coercion, unwanted sexual contact and other unwanted sexual experiences at some point in their lives (2). What’s heartbreaking is that this already too-high number goes up for lesbians (46.4%) and bisexual women (a staggering 74.9%) (3). And keep in mind that rape and sexual violence are some of the most underreported numbers we have (4). In Wisconsin alone, there were 5,609 injury hospitalizations and ER visits for women 15-44 because of intentional assault in 2014. In that same year, in one single day, Wisconsin domestic violence programs “provided services to 1,949 victims and had 367 requests for services that went unmet due to lack of resources” (5). In short: violence against women is not only still an issue but happening to a distressingly large percentage of American women. (I also want to take a quick moment to recognize that sexual and gender-based violence is not exclusive to women. This affects men as well and especially affects the LGBT+ and gender nonconforming communities. The fact that I chose to focus on women in this blog is not meant to detract from the realities of violence to these populations.)
So, how does the fact that almost half of all American women will experience some form of sexual violence victimization in their lifetime lead to the decision to eliminate all VAWA grant funds? Funds that Kim Gandy (President of the National Network to End Domestic Violence) said “is truly the foundation of our nation’s response to domestic and sexual violence, stalking and dating violence”(6)?
But this issue is about more than just numbers, shocking though they may be. Just volunteer your time at any local domestic violence shelter, sexual assault agency, or any other organizations that work with survivors [†]. Words cannot do justice to the experience of listening to their stories of pain and fear and the lifelong ramifications (higher levels of depression, suicide attempts, anxiety, PTSD, as well as poorer physical health) that come with their experiences of violence, as well as their successes in their personal journeys of healing (7). These women have been through so much and have fought so hard. They shouldn’t have to do it alone. They should have spaces like DAIS or theRape Crisis Center to go to for medical help, legal help, for shelter, and for empathy and support from those who understand.Then there’s the economics. The CDC estimates that intimate partner violence costs us $8.3 billion dollars a year (8). Each rape costs approximately $151,423 (9). Some of the best research we have identifies rape as our country’s most costly crime, at an annual cost of $127 billion (this is excluding child sexual abuse)(10). Yet we may be losing one of the only sources of federal funding that works to prevent these crimes- the 25 Office of VAW grants. These grants provide evidence-based direct services, intervention and assistance for victims of sexual assault as well as training and prevention programs. They cover everything from training law enforcement agencies to be more effective, trauma-informed responders, assisting with transitional housing for survivors, direct services to marginalized and underserved populations, providing legal assistance to survivors, and specifically supporting children, youth and elders experiencing violence and sexual assault (11). Without the critical, life-saving work of VAW grants, what is going to happen to the 74 million women who have or will experience some sort of sexual violence in their lifetimes(2)? We NEED these services. Many others have written about this (like this one, this one, or this one or even this one). But I truly believe this is an issue worth elevating at every opportunity. We need everyone to understand that so many women suffer in the United States but our current government wants to completely eliminate a huge source of federal funding.
Can we all at least agree that sexual assault and intimate partner violence (as two examples) remain a serious problem in the US? If the answer is yes, why would we eliminate the funding? In what world is that good math? In what world is that the humane choice? So YES. I’m angry. And you should be too.
1. Ellsberg M, Arango DJ, Morton M, et al. Prevention of violence against women and girls: what does the evidence say? Lancet (London, England). 2015; 385(9977):1555-66. doi:10.1016/s0140-6736(14)61703-7
2. Black MC, Basile, K.C., Breiding, M.J., Smith, S.G., Walters, M.L., Merrick, M.T., Chen, J., & Stevens, M.R. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control2011.
3. Center NSVR. Statistics About Sexual Violence2015.
4. Thomas E. Rape Is Grossly Underreported in the U.S., Study Finds. In: The Huffington Post. 2013.
http://www.huffingtonpost.com/2013/11/21/rape-study-report-america-us_n_4310765.html
. Accessed February 23 2017.
5. Violence NCAD. Domestic Violence National Statistics. In: NCADV, editor.2015. p. 2.
6. Gandy K. Intimate Partner Violence Report Proves VAWA Works. In: Post TH, editor. The Blog. The Huffington Post2012.
7. Carlson BE, Mcnutt L-A, Choi DY, et al. Intimate Partner Abuse and Mental Health
The Role of Social Support and Other Protective Factors. Violence Against Women. 2002; 8(6):720-45.
8. Prevention CfDCa. Intimate Partner Violence: Consequences. Atlanta, GA. 2015.
https://www.cdc.gov/violenceprevention/intimatepartnerviolence/consequences.html
. Accessed February 23 2017.
9. DeLisi M, Kosloski A, Sween M, et al. Murder by numbers: monetary costs imposed by a sample of homicide offenders. The Journal of Forensic Psychiatry & Psychology. 2010; 21(4):501-13.
10. Miller TR, Cohen MA, Wiersema B. Victim Costs and Consequences: A New Look. In: Justice UDo, editor.: Office of Justice Programs; 1996. p. 35.
11. Justice TUSDo. Grant Programs. United States DOJ. 2017.
https://www.justice.gov/ovw/grant-programs
. Accessed Feburary 23 2017.
As defined by the UN: gender-based violence is “physical, sexual or psychological harm or suffering to women, including threats of such acts, coercion or arbitrary deprivation of liberty, whether occurring in public or private life”
But really, you should probably look into volunteering because they are going to need all the help they can get if their programs are defunded.