The Physical Environment as a Social Determinant of Health: A Comprehensive Approach
Colleen Moran, MPH MS
Population Health Service Fellow
Division of Public Health
Bureau of Community Health Promotion
Bureau of Environmental & Occupational Health
Madison, Wisconsin
As Population Health Service Fellows, we’re always talking about the Social Determinants of Health (SDoH). It’s all about where we live, work, play and learn, right? But what if the physical environment of where we live, work, play and learn makes us sick? How big of a problem is this? Most of us are aware that contaminated environmental sources, such as water and air, can cause severe illness and even death. What about the more nuanced features of our physical environment like the structure of our neighborhoods? Recent research from the Urban Land Institute, Intersections: Health and the Built Environment[1] shows that:
- 13 million school days are missed each year in the U.S. due to asthma-related illnesses
- The number of children with type 2 diabetes has tripled since 1980;
- By 2030, it is anticipated that one out of 11 people in the U.S. will be at least 100 pounds overweight; and,
- Healthcare costs – the cost to treat illness, not keep people well — currently consumes 19 percent of the gross domestic product (GDP) of the United States; 9 percent of the GDP in Europe; and 5 percent of the GDP in China.
How Important is Environment?
These health
issues are all linked to the physical environment in which people live, work,
play and learn. Clearly this is a huge problem, a problem that calls for policy
and environmental change.
According to the Population Health Institute, County Health Rankings and Roadmaps[2]
model, approximately 10% of the upstream determinants of health are attributed
to our Physical Environment (environmental quality and the built environment).
The model attributes 40% of the SDoH to social and economic factors (e.g.,
education, employment, income, family and social support, and community
safety). Since the Physical Environment is so closely related to one's SES, dividing these two factors is not so simple.
I’m likely biased with a background in both public health and urban and regional planning, but to illustrate my point, consider the issue of neighborhood: your socio-economic status (SES) determines what sort of neighborhood you live in, whether or not there are sidewalks, parks, shade trees, a full service grocery store, a school within walking distance, a coffee shop, library, community center, etc. (of course some with the financial means to live in a place with these amenities may choose not to, but for the sake of this argument, we’re going to assume that is not the case). People with a lower SES are more likely to live in a physical environment that has a lack of all the aforementioned amenities plus the added negatives of features like factories, landfills, highways and the accompanying air and noise pollution. All of those physical environment features I just mentioned are determined by your SES.
I’m likely biased with a background in both public health and urban and regional planning, but to illustrate my point, consider the issue of neighborhood: your socio-economic status (SES) determines what sort of neighborhood you live in, whether or not there are sidewalks, parks, shade trees, a full service grocery store, a school within walking distance, a coffee shop, library, community center, etc. (of course some with the financial means to live in a place with these amenities may choose not to, but for the sake of this argument, we’re going to assume that is not the case). People with a lower SES are more likely to live in a physical environment that has a lack of all the aforementioned amenities plus the added negatives of features like factories, landfills, highways and the accompanying air and noise pollution. All of those physical environment features I just mentioned are determined by your SES.
How to Approach the Issue?
 I guess my argument really lies with
the issue of how we tackle the problem of dealing with how the physical
environment is a huge upstream determinant of health. Do we address it as a
discrete problem, putting in more bike lanes and sidewalks when and where we
can? Or do we treat it as the much more complex problem that it is? This would mean that when
we address issues with the physical environment, we recognize and work with the
issues surrounding SES and equity to ensure that we’re taking a comprehensive,
Socio-Ecologic Model (SEM) approach to dealing with these issues. This means using approaches that take into account the various levels of interaction in a person's life, from the intra personal to the policy level and everything in between.
I guess my argument really lies with
the issue of how we tackle the problem of dealing with how the physical
environment is a huge upstream determinant of health. Do we address it as a
discrete problem, putting in more bike lanes and sidewalks when and where we
can? Or do we treat it as the much more complex problem that it is? This would mean that when
we address issues with the physical environment, we recognize and work with the
issues surrounding SES and equity to ensure that we’re taking a comprehensive,
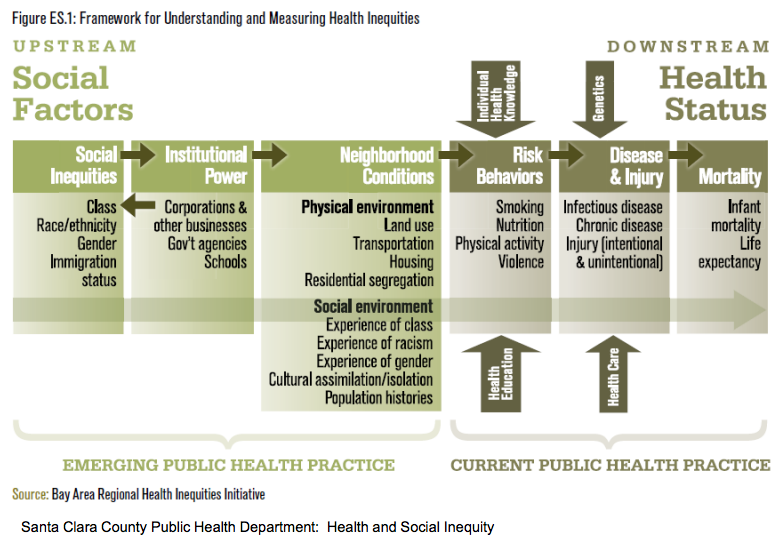
Socio-Ecologic Model (SEM) approach to dealing with these issues. This means using approaches that take into account the various levels of interaction in a person's life, from the intra personal to the policy level and everything in between. When we use the SEM, it is important to make sure that an equity component is incorporated. Are we looking at the upstream “isms” (e.g., classism, racism, sexism, etc.) and other social inequalities (sexual orientation, immigration status) as well as institutionalized power that has led to a disproportionate distribution of the negative aspects of the built environment (see figure right)?[3] How has "red-lining" affected the neighborhoods of many African Americans, how has immigration status affected the ability for families to live in a safe, healthy, vibrant community? Without asking these questions and getting at the true causes of these disparities associated with the physical environment, we're not really getting at the heart of the matter.
I would argue that if we’re not approaching how to deal with the Physical Environmental SDoH within these frameworks, then we’re only putting a band-aid on the problem. We can create a beautiful mixed used new urbanism neighborhood with sidewalks, trees, and bike infrastructure, but if we price out the individuals who used to live in that neighborhood (i.e., gentrification), have we really made progress towards improving our communities?
Moving Towards a Comprehensive Solution
A
recent editorial in the American Journal of Public Health argues that this targeting of impacted populations is one of the most pressing issues moving forward if we’re going to be
successful in creating healthier communities for all:
“[M]ore targeted attention to the most impacted
populations is needed. Public health and design professionals must recognize
those at greatest risk and with the greatest need for intervention and focus
accordingly. Those living in substandard housing, persons with no access to
safe places for physical activity, the elderly who cannot drive to their
destinations, urban children deprived of autonomy and nature contact, among
others, need to be at the center of built environment and health concerns.”[4]
So
what do we do about it? How do we tackle this huge issue of health inequities
in our physical environment? One start would be to use the approach of Health in All Policies (HiAP):
“…
an approach to improving the health of all people by incorporating health
considerations into collaborative decision-making across sectors and policy
areas (Rudolph et al., 2013). The goal of Health in All Policies is to ensure
that decision makers are informed about the health, equity, and sustainability
consequences of various policy options during the policy development process
(California Health in All Policies Task Force, 2010a).”[5]
One key piece of HiAP that I think is
crucial is the, “collaborative decision-making across sectors and policy areas” [6] piece. Public health needs
to continue to ramp up its efforts to work intersectorally with urban and
regional planners, transportation planners and engineers, economic development,
housing authorities, and all other sectors involved in shaping our physical
environment. An interesting infographic, “Better Transportation
Options=Healthier Lives,”
created by the Robert Wood Johnson Foundation echoes this sentiment:
“Decisions
about transportation and community development at the community, state and
national level should all take health impacts into account. Transportation,
planning and public health professionals can work together to create healthier
communities”[7]
All of this collaboration of course, must
occur within a health equity framework. This collaboration involves huge systems level issues and I don't for a second pretend that any of this will be easy or that it will occur quickly. It will be hard work and it will take time. But, if we continue to move ahead with these
overarching HiAP, health equity concepts in mind, which I think we’re perfectly
poised to do, I am optimistic that we can create healthier, more equitable
communities for all.
[3]
Bay Area Regional Health Inequalities Initiative. Framework for Understanding
and Measuring Health Inequalities. Santa Clara County Health Dept.
[4] Jackson
J., Dannenberg, A., Frumkin H. Health and the Built Environment: 10 Years
After. American Journal of Public
Health | September 2013, Vol 103, No. 9
[5]
Rudolph L., Caplan J., Mitchell C., Ben-Moshe
K., and Dillon L. Health in All Policies: Improving Health Through Intersectoral
Collaboration. IOM, September 18, 2013.
[6]
Rudolph L., Caplan J., Mitchell C., Ben-Moshe
K., and Dillon L. Health in All Policies: Improving Health Through Intersectoral
Collaboration. IOM, September 18, 2013.
[7] Better Transportation Options=Healthier Lives.
New Public Health. Robert Wood Johnson Foundation. http://www.rwjf.org/en/blogs/new-public-health/2012/10/better_transportatio.html